Organ-Specific Medicine Laboratory
Department of Surgical Oncology, Transplant Surgery and General Surgery
Faculty of Medicine
Faculty of Medicine
As a part of the “Excellence Initiative – Research University” program, a new core facility – the Organ-Specific Medicine Laboratory – is starting operations at the Medical University of Gdansk. The unit was created thanks to the experience of the staff at the Department of General, Endocrine and Transplant Surgery, and the Department of Oncological Surgery, which were established within the structure of the Faculty of Medicine.
OUR POTENTIAL
- freezer: up – 80 degr. C
- stock of liquid nitrogen + Dewar flas
- centrifuges – 2 Hettich EBA 200 units, and an older model (up to 6000 RPM)
- ultrasound scanners – 3 units, two full-size, high-quality ultrasound scanners, and one POCUS (point-of-care) devic
- laparoscopic columns, including those with ICG imaging
- ICG imaging camera (for open surgeries)
- laser Doppler scanner
- gamma camer
- neuromonitoring
SCOPE OF SERVICES
The Organ-Specific Medicine Laboratory care facility provides access to clinical expertise and facilitates access to patients, including tissue and clinical data, for MUG, FarU and external collaborators.
Scope of activities conducted:
- recruitment of patients from specific clinical areas for basic research and clinical trials
- designing/consulting on the design of research studies involving patients for MUG colleagues and external collaborators
- conducting non-commercial and commercial clinical trials
- collecting, cataloguing and freezing tissue samples from patients
- collecting, cataloguing and transferring patients’ blood samples to the laboratory
- collecting clinical information on patients
- analysis of clinical data of patients for scientific resear
- interpreting the clinical context of scientific findings
The foregoing capabilities of the Core Facility enable a translational approach to science, and will improve collaboration between MUG and external units. The Core Facility provides access not only to patient-obtained biological samples and clinical data, but more importantly: to experts who support study planning and result interpretation in a clinical context.
Clinical areas of the Core Facility
Clinical areas are reflected by the organizational structure of the Department of Oncology, Transplantation and General Surgery, which operates at UCK (Fig. 1).
Clinical activities conducted include:
- patients with acute abdominal conditions (about 100-200 per year)
- patients with hernias (about 50 per year)
- patients with liver failure of various etiologies (toxic, autoimmune, post-inflammatory) undergoing liver qualification and transplantation (about 50 per year)
- patients with kidney failure undergoing kidney transplantation (about 100 per year)
- patients with benign and malignant diseases of the bile ducts, gallbladder and liver undergoing surgery (about 50-100 per year) and locoregional treatment(about 250 per year)
- patients with benign and malignant pancreatic diseases undergoing resection surgery (about 50 per year)
- morbidly obese patients undergoing bariatric surgery (about 200 per year)
- patients with upper gastrointestinal tract cancers (of the esophagus and the stomach) undergoing resection procedures (about 30 per year)
- patients with unresectable upper gastrointestinal tumors subjected to parenteral and enteral nutrition (about 50 per year)
- colorectal cancer patients undergoing resection surgery (approximately 200 per year)
- patients with proctological diseases undergoing topical treatment (approx. 1000 per year)
- patients with malignant and benign thyroid diseases undergoing resection procedures (about 250 per year)
- patients with malignant and benign adrenal diseases undergoing resection procedures (about 50 per year)
- patients with malignant breast diseases undergoing resection surgery (approx. 400 per year)
- patients with malignant soft tissue diseases (melanomas and sarcomas) undergoing resection procedures (about 50 per year)
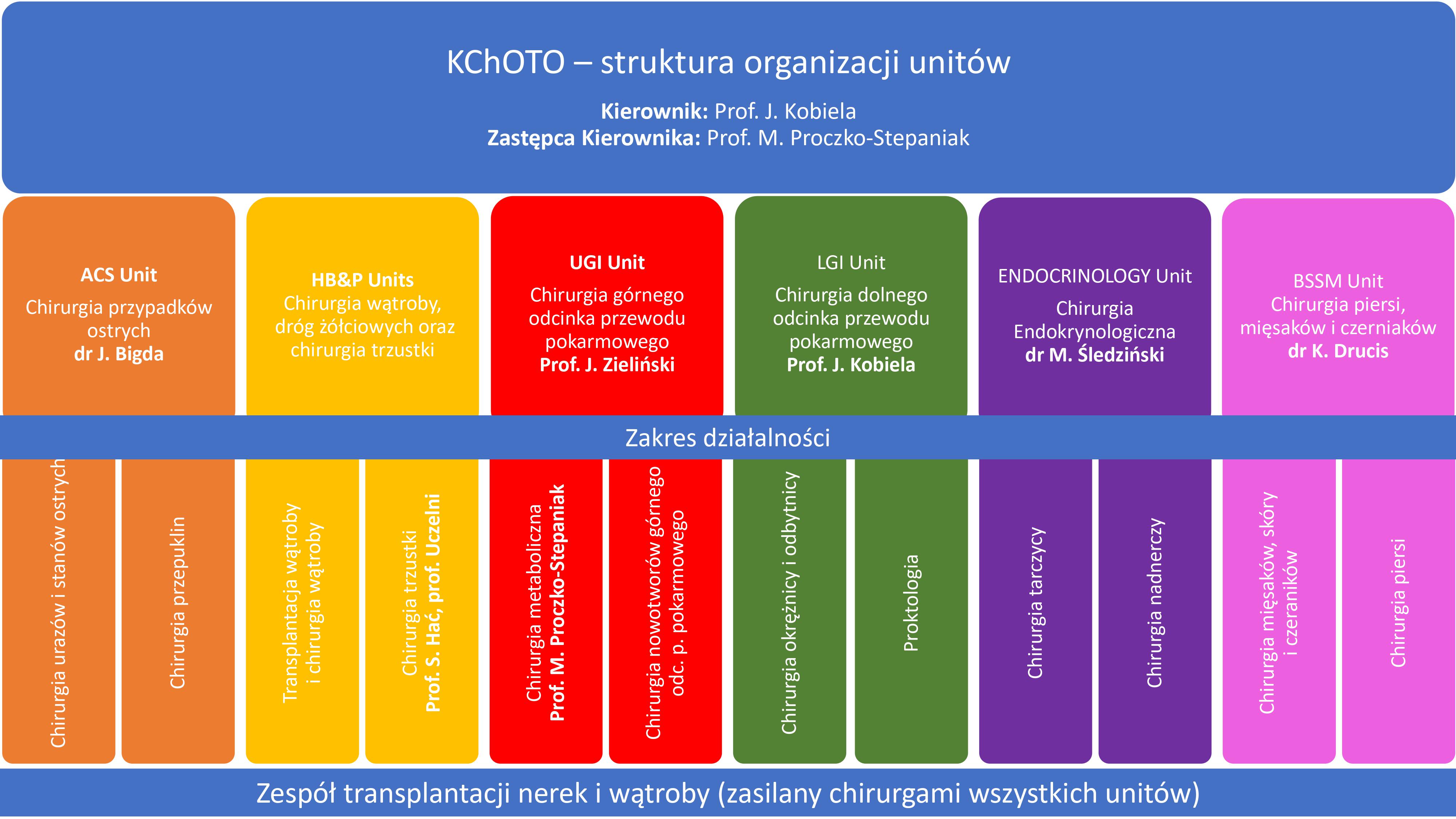 Fig. 1
Fig. 1
RESEARCH TEAM
The Core facility has a number of experts with extensive clinical and scientific experience:
- Prof. Jarosław Kobiela – expert in colorectal surgery and colorectal cancer
- Prof. Michał Kamiński – expert in internal medicine, gastroenterology and clinical oncology
- Nastazja Pilonis, Ph.D. – expert in gastroenterology and screening
- Justyna Bigda, Ph.D. – expert in hernia and acute hernia surgery and kidney transplantation surgery
- Prof. Stanisław Hać – expert in pancreatic surgery
- Justyna Kostro, Ph.D. – expert in kidney transplantation and access to renal replacement therapy
- Prof. Jacek Zieliński – expert on upper gastrointestinal tract tumors
- Prof. Monika Proczko-Stepaniak – expert in the surgical treatment of morbid obesity – bariatric surgery
- Maciej Śledziński, Ph.D. – expert in endocrine surgery
- Andrzej Hellmann, Ph.D. – expert in endocrine surgery
- Kamil Drucis, Ph.D. – expert in breast surgery, melanomas, and sarcomas
- Małgorzata Nowosad, Ph.D. – expert in liver surgery and liver transplantation
- Piotr Domagała, Ph.D. – expert in kidney and liver transplantation
- Wojciech Polak, Ph.D. – expert in general surgery, clinical transplantology and vascular surgery
- Piotr Spychalski, Ph.D. – expert in scientific research methodology in clinical sciences
- Magda Rybicka-Misiejko, Ph.D. – expert in genetic diagnosis of cancer using modern methods of molecular biology
- Małgorzata Bagnucka, M.A. – scientific and technical coordinator
- Michał Bystram, M.A. – scientific and technical coordinator
- nurses with experience in participating in commercial and non-commercial clinical trials
PUBLICATIONS
Publications that have been developed by using the research methods described:
1. Spychalski, P. et al. Adenoma to Colorectal Cancer Estimated Transition Rates Stratified by BMI Categories-A Cross-Sectional Analysis of Asymptomatic Individuals from Screening Colonoscopy Program. Cancers (Basel) 14, (2021).
2. Girnyi, S., Ekman, M., Marano, L., Roviello, F. & Połom, K. Complete Mesogastric Excisions Involving Anatomically Based Concepts and Embryological-Based Surgeries: Current Knowledge and Future Challenges. Curr Oncol 28, 4929-4937 (2021).
3. Czaja-Stolc, S. et al. Adherence to Caloric and Protein Recommendations in Older Hemodialysis Patients: A Multicenter Study. Nutrients 14, (2022).
4. Wilczyński Maciej Jakub. Analiza klinicznych i metabolicznych efektów One Anastomosis Gastric Bypass: praca doktorska. (Gdański Uniwersytet Medyczny, 2022).
5. Łabul, M. et al. Analysis of the Factors Contributing to Bariatric Success After Laparoscopic Redo Bariatric Procedures: Results from Multicenter Polish Revision Obesity Surgery Study (PROSS). Obes Surg 32, 3879-3890 (2022).
6. Hellmann, A. R., Szymański, M., Śledziński, M., Biernat, W. & Preis-Hellmann, A. ‘Ancient’ Schwannoma of the adrenal gland pretending to be melanoma metastasis. Pol Arch Intern Med 132, 16260 (2022).
7. Reczkowicz, J. et al. Bariatric Surgery Induced Changes in Blood Cholesterol Are Modulated by Vitamin D Status. Nutrients 14, (2022).
8. Kozak Oliwia, Hać Stanisław, Pieńkowska Joanna, & Studniarek Michał. Benefitial role of electrochemotherapy in locally advanced pancreatic cancer radiological perspective. Pol. J. Radiol. 87, e30-e42 (2022).
9. Hliwa, A. et al. Changes in the Serum Fatty Acid Profile After Anhepatic Phase of Orthotopic Liver Transplantation Procedure. Front Physiol 13, 817987 (2022).
10. Kraszewski Jakub, Stefaniak Tomasz, Kobiela Jarosław, & Spychalski Piotr. Chirurgia onkonarządowa – przyszłość chirurgii onkologicznej. Gazeta GUMed 50-52 (2022).
11. Wilczyński, M. et al. Comparison of the Long-term Outcomes of RYGB and OAGB as Conversion Procedures After Failed LSG – a Case-Control Study. J Gastrointest Surg 26, 2255-2265 (2022).
12. Filipowicz, N. et al. Comprehensive cancer-oriented biobanking resource of human samples for studies of post-zygotic genetic variation involved in cancer predisposition. PLoS One 17, e0266111 (2022).
13. Potrykus, M., Czaja-Stolc, S., Małgorzewicz, S., Proczko-Stepaniak, M. & Dębska-Ślizień, A. Diet Management of Patients with Chronic Kidney Disease in Bariatric Surgery. Nutrients 15, (2022).
14. Hellmann Andrzej, Śledziński Maciej, Cytawa Wojciech, & Wiśniewski Piotr. Does Hashimoto’s affect the course of papillary thyroid cancer? Based on patients group with high incidence of HT in PTC. vol. 73, supl. A, s. 7 (2022).
15. Łącka Monika & Hać Stanisław. Duodenal diverticulum perforation mimicking acute cholecystitis – case reports and a literature review. Eur. J. Transl. Clin. Med 64-70 (2022).
16. Szymański, M. et al. Evaluation of esophageal pathology in a group of patients 2 years after one-anastomosis gastric bypass (OAGB) – Cohort study. _Obes Res Clin Pract_16, 82-86 (2022).
17. Proczko, M. et al. Evolution of the body image perception of people with obesity on the pathway from bariatric surgery to body contouring lift surgery. J Plast Reconstr Aesthet Surg 75, 860-869 (2022).
18. Sass, P. et al. Examination of epigenetic inhibitor zebularine in treatment of skin wounds in healthy and diabetic mice. J Tissue Eng Regen Med 16, 1238–1248 (2022).
19. Cwalinski, T. et al. Fluorescence Imaging Using Methylene Blue Sentinel Lymph Node Biopsy in Melanoma. Surg Innov 29, 503-510 (2022).
20. Patel, A., Spychalski, P. & Kobiela, J. For and Against Routine Removal of Peripheral Intravenous Catheters. JAMA Intern Med 182, 457 (2022).
21. Szymański, M., Hellmann, A., Jelitto, M., Kaska, Ł. & Proczko-Stepaniak, M. Gastrointestinal tract necrosis caused by severe foodborne botulism. Pol Arch Intern Med 132, 16251 (2022).
22. Singhal, R. et al. Handling of the Covid-19 Pandemic and Its Effects on Bariatric Surgical Practice: Analysis of GENEVA Study Database. Obes Surg 32, 3908–3921 (2022).
23. Gołębiewska Martyna, Piątek Olga, Kuziemski Krzysztof, & Stefaniak Tomasz. Impact of persistent coronavirus infection on the treatment of an immunocompromised oncological patient. Palliat. Med. Pract 16, 183-186 (2022).
24. Potrykus Marta, Szymański Michał, Kaska Łukasz, & Janczy Agata. Intestinal barrier disorders and metabolic endotoxemia in obesity: current knowledge. Post. Hig. Med. Dośw. 76, 71–80 (2022).
25. Przybył, A. et al. Kidney Re-Transplantation after Simultaneous Heart and Kidney Transplant: Case Study and Literature Review. Transplantology 3, 124-129 (2022).
26. Rudziński, M. et al. Kidney stones are common in patients with short-bowel syndrome receiving long-term parenteral nutrition: A predictive model for urolithiasis. JPEN J Parenter Enteral Nutr 46, 671-677 (2022).
27. Kostro, J. Z. et al. Kidney Transplantation in Patients After Bariatric Surgery: High-Volume Bariatric and Transplant Center Experience. Transplant Proc 54, 955-959 (2022).
28. Śledziński Maciej et al. Lobectomy for the treatment of thyroid cancer – outcomes of implementation of the 2018 Polish consensus in a single center. (2022).
29. Wójtowicz Katarzyna. Moja przygoda z pielęgniarstwem onkologicznym. Gazeta GUMed 42-43 (2022).
30. Ekman, M. et al. Near-Infrared Fluorescence Image-Guided Surgery in Esophageal and Gastric Cancer Operations. Surg Innov 29, 540–549 (2022).
31. Stefaniak Tomasz & Tybińkowska Anna. Nowoczesny ordynator: wybitny klinicysta czy Q-menedżer? Menedż. Zdr. 40-42 (2022).
32. Zalewska, E. et al. Oncogenic osteomalacia – detection of the tumour site upon physical examination. Endokrynol Pol 73, 792-793 (2022).
33. Liakh, I. et al. One-anastomosis gastric bypass modulates the serum levels of pro- and anti-inflammatory oxylipins, which may contribute to the resolution of inflammation. Int J Obes (Lond) 46, 408-416 (2022).
34. Dobrzycka, M., Bzoma, B., Bieniaszewski, K., Dębska-Ślizień, A. & Kobiela, J. Pretransplant BMI Significantly Affects Perioperative Course and Graft Survival after Kidney Transplantation: A Retrospective Analysis. J Clin Med 11, (2022).
35. Czaja-Stolc, S., Potrykus, M., Stankiewicz, M., Kaska, Ł. & Małgorzewicz, S. Pro-Inflammatory Profile of Adipokines in Obesity Contributes to Pathogenesis, Nutritional Disorders, and Cardiovascular Risk in Chronic Kidney Disease. Nutrients 14, (2022).
36. Szymański Michał. Rola badań dodatkowych ze szczególnym uwzględnieniem endoskopii w ocenie ryzyka i leczeniu powikłań w grupie pacjentów operowanych z powodu otyłości chorobliwej: praca doktorska. (Gdański Uniwersytet Medyczny, 2022).
37. Liakh, I., Proczko-Stepaniak, M., Sledzinski, M. & Mika, A. Serum free fatty acid levels and insulin resistance in patients undergoing one-anastomosis gastric bypass. Wideochir Inne Tech Maloinwazyjne 17, 194-198 (2022).
38. Patel, A., Spychalski, P. & Kobiela, J. Short-course radiotherapy and consolidation chemotherapy: in search of a balanced protocol. Br J Surg 109, e50-e51 (2022).
39. Stefaniak Tomasz & Tybińkowska Anna. Spotkanie BQMM: co to i po co? Menedż. Zdr. 73-77 (2022).
40. Peplinska-Miaskowska, J., Wichowicz, H., Smoleński, R., Jablonska, P. & Kaska, L. The comparison of nucleotide metabolites and amino acids patterns in patients with eating disorders, with and without symptoms of depression. Nucleosides Nucleotides Nucleic Acids 41, 333-341 (2022).
41. Śledziński, M., Hliwa, A., Gołębiewska, J. & Mika, A. The Impact of Kidney Transplantation on the Serum Fatty Acid Profile in Patients with End-Stage Kidney Disease. Nutrients 14, (2022).
42. Mizera, M. et al. The impact of severe postoperative complications on outcomes of bariatric surgery-multicenter case-matched study. Surg Obes Relat Dis 18, 53-60 (2022).
43. Mika, A. et al. The impact of the interplay of the intestinal microbiome and diet on the metabolomic and health outcomes of bariatric surgery. Obes Rev 23, e13455 (2022).
44. Wiśniewski Piotr, Hellmann Andrzej, Jendrzejewski Jaroslaw, Cytawa Wojciech, & Kowalski Jacek. The risk of malignancy in Bethesda IV thyroid nodules in Poland is low – time to slow down the rush to surgery. in (2022).
45. Meyer-Szary, J. et al. The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals-Cross-Sectional Multispecialty Review. Int J Environ Res Public Health 19, (2022).
46. Pęksa, R. et al. Tumor Budding Is an Independent Prognostic Factor in Pancreatic Adenocarcinoma and It Positively Correlates with PD-L1 Expression on Tumor Cells. Biomedicines 10, (2022).
47. Antoszewska Magdalena, Spychalski Piotr, & Barańska-Rybak Wioletta. Zastosowanie pomiaru bioimpedancji w procesie gojenia się owrzodzenia u pacjenta z cukrzycą typu 1. in vol. t. 8, nr 4 159 (2022).
48. Czerwiec, K. et al. Adipose-Derived Mesenchymal Stromal Cells in Basic Research and Clinical Applications. Int J Mol Sci 24, (2023).
49. Hellmann, A. et al. Alterations in the amino acid profile in patients with papillary thyroid carcinoma with and without Hashimoto’s thyroiditis. Front Endocrinol (Lausanne) 14, 1199291 (2023).
50. Palus, D. K. et al. Analysing COVID-19 treatment outcomes in dedicated wards at a large university hospital in northern Poland: a result-based observational study. BMJ Open 13, e066734 (2023).
51. Wysocki, M. et al. Analysis of the risk factors for perioperative morbidity after laparoscopic revisional bariatric procedures: results from the multicenter Polish Revision Obesity Surgery Study. Surg Obes Relat Dis 19, 68-75 (2023).
52. Janczy, A. et al. Assessment of nutritional and low-grade inflammation status among bariatric surgery candidates in the preoperative period during the COVID-19 pandemic. Obes Res Clin Pract 17, 275-278 (2023).
53. Dowgiałło-Gornowicz, N., Lech, P. & Major, P. Bariatric and Metabolic Surgery in Patients Older than 65 Years – a Multicenter Study. Obes Surg 33, 3106-3111 (2023).
54. Medas, F. et al. Effect of the COVID-19 pandemic on surgery for indeterminate thyroid nodules (THYCOVID): a retrospective, international, multicentre, cross-sectional study. Lancet Diabetes Endocrinol 11, 402-413 (2023).
55. Janczy, A. et al. Increased Amount of Polyunsaturated Fatty Acids in the Intestinal Contents of Patients with Morbid Obesity. Obes Surg 33, 1228-1236 (2023).
56. Placzke, J. et al. Modern Approach to Melanoma Adjuvant Treatment with Anti-PD1 Immune Check Point Inhibitors or BRAF/MEK Targeted Therapy: Multicenter Real-World Report. Cancers (Basel) 15, (2023).
57. Dudzic, W. et al. Nutritional Status and the Outcomes of Endoscopic Stenting in Benign and Malignant Diseases of Esophagus. Nutrients 15, (2023).
58. Dowgiałło-Gornowicz, N. et al. Predictors of complete remission of type 2 diabetes in patients over 65 years of age – a multicenter study. Obes Surg 33, 2269-2275 (2023).
59. Dzierżyńska, M. et al. Release systems based on self-assembling RADA16-I hydrogels with a signal sequence which improves wound healing processes. Sci Rep 13, 6273 (2023).
60. Dowgiałło-Gornowicz, N., Janik, M., Lech, P., Kowalski, G. & Major, P. Revisional bariatric surgery after adjustable gastric band: a multicenter Polish Revision Obesity Surgery Study (PROSS). BMC Surg 23, 94 (2023).
61. Pakiet, A. et al. Serum fatty acid profiles in breast cancer patients following treatment. BMC Cancer 23, 433 (2023).
62. Lange, O., Proczko-Stepaniak, M. & Mika, A. Short-Chain Fatty Acids-A Product of the Microbiome and Its Participation in Two-Way Communication on the Microbiome-Host Mammal Line. Curr Obes Rep 12, 108-126 (2023).
63. Wysocki, M. et al. The analysis of factors increasing the odds for type 2 diabetes mellitus remission following re-do bariatric surgery after laparoscopic sleeve gastrectomy- cohort study. Langenbecks Arch Surg 408, 371 (2023).
64. Sobocki, J. et al. The Association of Polish Surgeons (APS) clinical guidelines for the use of laparoscopy in the management of abdominal emergencies. Part I. Wideochir Inne Tech Maloinwazyjne 18, 187-212 (2023).
65. Ziętek, M. et al. The Current Treatment Trends and Survival Patterns in Melanoma Patients with Positive Sentinel Lymph Node Biopsy (SLNB): A Multicenter Nationwide Study. Cancers (Basel) 15, (2023).
66. Spychalski, P. & Kobiela, J. The obesity phenomenon in colorectal cancer. Colorectal Dis 25, 1535-1536 (2023).\
67. Łukasiewicz, M., Śledziński, M., Szymański, M., Kowalski, J. & Hellmann, A. Therapeutic challenge: a giant, infiltrating intrathyroidal thymic carcinoma of the thyroid gland. Pol Arch Intern Med 133, 16475 (2023).
68. Bes, M., Chojnacka, I., Szczecińska, W. & Zieliński, J. Treatment of Fournier’s gangrene with negative pressure wound therapy in the course of sepsis – Case report. Int J Surg Case Rep 110, 108641 (2023).
CONTACT

Mail piotr.spychalski@gumed.edu.pl

Mail malgorzata.bagnucka@gumed.edu.pl

Mail michal.bystram@gumed.edu.pl
Division of General, Endocrine and Transplant Surgery
Medical University of Gdańsk
Mariana Smoluchowskiego 17 Steet
80-214 Gdańsk
Phone 58 349 30 10 (Secretariat)