Translational Medicine Centre
ABOUT US
The Translational Medicine Centre (TMC) is a core-facility, that has been established in 2019, to pursue transdisciplinary projects in which the evaluation of cardiovascular structure and function may have cognitive and clinical relevance. The research conducted in our Centre includes standard and innovative methods of evaluating the cardiovascular system on its every level, i.e. starting from echocardiographic imaging of the heart, through the assessment of the function of great vessels (pulse wave propagation within the aorta, dilation of cerebral arteries) to the functional and structural evaluation of microcirculation. It is the microcirculation that is the focus of recent global research trends in a range of cardiovascular conditions, diseases outside of cardiometabolic medicine, and studies evaluating the safety of drugs and nutraceuticals.
OUR MISSION
Comprehensive studies of cardiovascular regulation and disease pathophysiology go beyond the evaluation of target structures, i.e., the heart and vessels. With this fact in mind, our Centre also offers the opportunity to evaluate the autonomic nervous control of both breathing and circulation, i.e. two inseparable systems that share common regulatory mechanisms. The selection of research methods available at the Translational Medicine Centre was preceded by numerous consultations with experts in individual fields from our University as well as experts from outside the Medical University of Gdańsk. The consultation aimed to develop an optimal model for acquiring a comprehensive cardiovascular phenotype far beyond standard clinical assessment. The data acquired in our core-facility will not only enable the research priorities described in our University’s IDUB application, but will also determine a new standard for the holistic assessment of the heart and vasculature in relation to organ damage.
RESEARCH PROFILE
Our research armamentarium involves standard methods used in clinical medicine, methods that are unique nationwide, as well as world specialist methods listed below:
1. Pressure assessment of arterial values:
- indirect oscillometric blood pressure measurement (Omron M3 sphygmomanometer, Omron Intellisense 7), (STANDARD);
- continuous non-invasive blood pressure measurement Finometer ®;
- 24-hour out-patient indirect blood pressure measurement SpaceLabs 90207 – evaluation of mean arterial pressure, evaluation of pulse pressure, evaluation of blood pressure variability including evaluation of daily blood pressure profile, (STANDARD).
2. 12-lead ECG, Multicard E 300 with digital recording, (STANDARD).
3. 24-hour out-patient ECG (Holter) recording, (STANDARD).
4. Analysis of heart rate variability (‘HRV’) and baroreceptor reflex sensitivity (‘BRS’) in 15-minute recordings (Finometer, PowerLab).
5. Transthoracic echocardiography (GE VIVID E95): acquisition of images and offline analysis using the EchoPac workstation. Assessment of the structure and function of the heart using one-dimensional, two-dimensional, four-dimensional imaging, Doppler techniques (continuous wave and pulsed wave Doppler, color Doppler, tissue Doppler) and speckle tracking analysis (LV strain and strain rate).
6. Non-invasive tonometric assessment of arterial compliance, pulse wave velocity analysis (carotid-femoral) and non-invasive central pressure assessment – SphygmoCor XCEL System, (EXTENDED STANDARD); XCEL is a non-invasive tool for clinical assessment of central pressure. The central aortic pressure curve is obtained from pulsations recorded noninvasively over the brachial artery using an arm cuff to measure blood pressure. The analysis of the obtained curve enables the calculation of key parameters such as systolic central arterial pressure, central pulse pressure, and parameters that assess vascular stiffness such as augmentation pressure and augmentation index (AIx). The SphygmoCor XCEL system also measures the rate of pulse wave propagation (blood pressure) in the aorta from the ascending aorta to the femoral artery. The rate of pulse wave propagation is assessed by the pulse measured noninvasively, simultaneously over the carotid and femoral arteries. The examination is performed in a supine position using a tonometer, a special pen-like device applied around the carotid artery, and a blood pressure cuff worn around the thigh on the femoral artery to assess the deformation of the arterial vessels. Measuring the distance between pulse wave recording locations allows the system to calculate the speed of pulse wave travel.
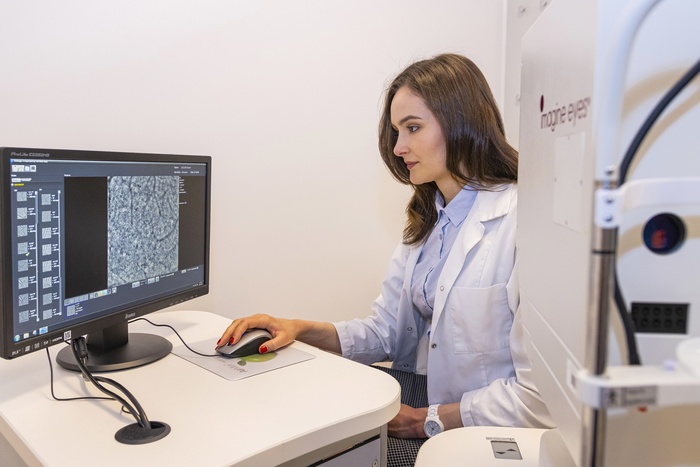
7. A non-invasive examination of retinal microcirculation with the use of a scanning laser Doppler flowmeter with automatic full-field perfusion imaging analysis (AFFPIA), which allows precise assessment of retinal vessels in particular: a structure of retinal arteries, remodelling features based on the analysis of outer and inner vessel diameter, assessment of wall-to-lumen ratio, wall thickness and wall cross-sectional area (volume of vascular wall per unit length) of retinal arteries.
8. A non-invasive examination of cutaneous microcirculation using AngioTester (SN-2016-009M, Angionica, Łódź, Poland), which involves is the assessment of flow mediated skin fluorescence (FMSF). The essence of FMSF is to monitor the fluorescence of dihydronicotinamide adenine dinucleotide (NADH), the content of which changes secondary to brachial artery occlusion (3-minute occlusion using an arm blood pressure cuff). The FMSF technique enables the assessment of microcirculatory function in the post-occlusion period as well as the observation of biochemical processes occurring in the examined tissue during controlled ischaemia. The FMSF technique enables the analysis of multiple parameters of the NADH fluorescence curve, the most relevant of which are (1) the ischaemic response (IRmax) and (2) the hyperemic response (HRmax). IRmax is the percentage increase in NADH fluorescence relative to baseline recorded during vessel occlusion.
9. Non-invasive assessment of cutaneous microcirculation based on laser speckle contrast imaging (LSCI) analysis. LSCI is a research technique that allows non-invasive, non-contact, real-time monitoring of changes in microcirculatory perfusion. LSCI has excellent measurement repeatability as well as very good temporal and spatial resolution. The LSCI technique enables the analysis of changes in the perfusion curve, including a detailed analysis of the response to stimuli; here, the PORH test (post-occlusive reactive hyperemia; three-minute brachial artery occlusion using an indirect blood pressure cuff – a test performed concurrently with the FMSF test described in section no. 11). During the PORH test, the most significant factors are the percentage increase in microcirculatory flow recorded after vessel occlusion compared to resting flow (%BL), time to peak flow, and area under the curve for the entire duration of the congestive response (AUC). The PORH test allows the assessment of endothelium-dependent vasodilatory potential of microcirculation.
10. Indirect assessment of cerebral microcirculation based on the measurement of subarachnoid arterial blood flow (cc-TQ) using a non-invasive method of Near Infrared Transillumination – Back Scattering Sounding (NIR-T/BSS); NIR-T/BSS studies have been performed at the Medical University of Gdańsk for several years, e.g. in the Department of Human Physiology of the Faculty of Health Sciences, and the Department of Hypertension and Diabetology of the Faculty of Medicine.
11. Non-invasive ultrasound assessment of common carotid artery function (dilation) and morphology (multiarray-tracking, ArtLab system, Esaote), (EXTENDED STANDARD).
12. Non-invasive ultrasound assessment of cerebral vascular blood flow by measuring changes in blood flow velocity (systolic, diastolic, and mean), resistivity and pulsatility index, and middle cerebral artery acceleration time using transcranial Doppler (TCD) effect, (STANDARD).
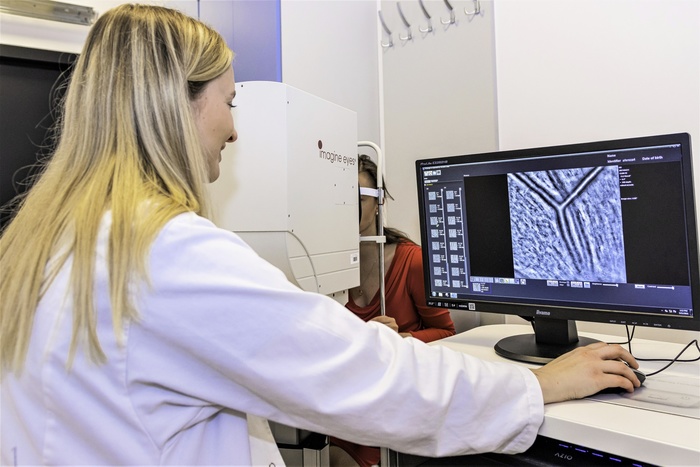
13. Non-invasive assessment of vascular and cone structures evaluated with a retinal camera using adaptive optics (Rtx-1e); an image acquisition technique that uses a floating mirror system allows unique resolution and repeatability/reproducibility of re-evaluation of the same anatomical regions of the posterior pole of the eye. In addition, Rtx-1e enables quantitative assessment of the cone density of selected regions of the macula.
14. Actigraphy – measurement of motor activity using ActiWatch 2 and MotionWatch 8 apparatus. Actigraphic recording is a non-invasive method used in the diagnosis of sleep-wake rhythm disorders, insomnia, hypersomnia, sleep apnea, etc. The method in its simplified version has been massively popularized in everyday use (practically every smartphone has a built-in accelerator and enables e.g. an estimation of a daily number of steps / distances covered; and with the use of applications installed in the phone also semi-quantitative and qualitative estimation of sleep), (STANDARD).
15. Non-invasive ambulatory polygraphy (clinical standard for the assessment of breathing disorders during sleep). The examination consists in non-invasive recording of respiratory movements with the use of elastic belts worn on the chest and abdomen: induction or with the use of a belt with a piezoelectric sensor, pulse oximetry measurement and measurement of airflow through the nose with the use of a nasal cannula and body position during the recording. The examination lasts all night, (STANDARD).
In order to maintain the highest research standards, we also take care to disseminate the results of reproducibility and repeatability tests of the acquired data. This procedure is indispensable when using cardiovascular assessment techniques that rely on the experience and competence of the investigators (e.g. subjective analyses of sonographic images).
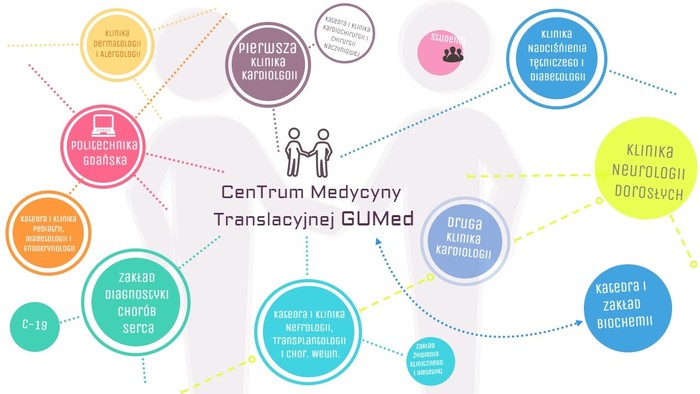
SCIENTIFIC COOPERATION (CMT)
OUR TEAM (CMT)
- Prof. Dr. Habil. Krzysztof Narkiewicz,M.D., Chairman of the Scientific Council of the TMC
- Dr. Habil. Jacek Wolf, M.D., CMT Coordinator
- Prof. Dr. Habil. Marcin Hellmann, M.D.
- Magdalena Dzitkowska, Ph.D.
- Edyta Kowalczys-Dąbrowska, Ph.D.
- Natasza Malinowska, Ph.D.
- Magdalena Chmara, Ph.D.
- Wiesława Kucharska, certified nurse
- Junior Specialist Dalia Trzonek
- Junior Specialist Sonia Trawińska
- Junior Specialist Aleksandra Michnowska

OUR PUBLICATIONS
1. Unilateral Carotid Body Resection in Resistant Hypertension: A Safety and Feasibility Trial.
Narkiewicz K, Ratcliffe LE, Hart EC, Briant LJ, Chrostowska M, Wolf J, Szyndler A, Hering D, Abdala AP, Manghat N, Burchell AE, Durant C, Lobo MD, Sobotka PA, Patel NK, Leiter JC, Engelman ZJ, Nightingale AK, Paton JF. JACC Basic Transl Sci. 2016 Aug 29;1(5):313-324
2. Effect of beta-blocker therapy on heart rate response in patients with hypertension and newly diagnosed untreated obstructive sleep apnea syndrome.
Wolf J, Drozdowski J, Czechowicz K, Winklewski PJ, Jassem E, Kara T, Somers VK, Narkiewicz K. Int J Cardiol. 2016 Jan 1;202:67-72.
3. Pial artery and subarachnoid width response to apnoea in normal humans.
Wszedybyl-Winklewska M, Wolf J, Swierblewska E, Kunicka K, Gruszecki M, Guminski W, Winklewski PJ, Frydrychowski AF, Bieniaszewski L, Narkiewicz K.J Hypertens. 2015 Sep;33(9):1811-7;
4. Lumen narrowing and increased wall to lumen ratio of retinal microcirculation are valuable biomarkers of hypertension-mediated cardiac damage.
Dąbrowska E, Harazny JM, Miszkowska-Nagórna E, Stefański A, Graff B, Kunicka K, Świerblewska E, Rojek A, Szyndler A, Wolf J, Gruchała M, Schmieder RE, Narkiewicz K.Blood Press. 2019 Sep 5:1-10
5. Aortic stiffness is not only associated with structural but also functional parameters of retinal microcirculation.
Dąbrowska E, Harazny JM, Miszkowska-Nagórna E, Stefański A, Graff B, Kunicka K, Świerblewska E, Rojek A, Szyndler A, Gąsecki D, Wolf J, Gruchała M, Laurent S, Schmieder RE, Narkiewicz K.Microvasc Res. 2020 May;129:103974
6. Current understanding of the effects of inspiratory resistance on the interactions between systemic blood pressure, cerebral perfusion, intracranial pressure, and cerebrospinal fluid dynamics.
Winklewski PJ, Wolf J, Gruszecki M, Wszedybyl-Winklewska M, Narkiewicz K.J Appl Physiol (1985). 2019 Nov 1;127(5):1206-1214
7. The phenomenon of HbA1c stability and the risk of hypoglycemia in long-standing type 1 diabetes.
Wolnik B, Orłowska-Kunikowska E, Błaszkowska M, Graff B, Wolf J, Czupryniak L, Narkiewicz K.Diabetes Res Clin Pract. 2019 Jun;152:96-102
8. Prevalence and distribution of left ventricular diastolic dysfunction in treated patients with long-lasting hypertension.
Świerblewska E, Wolf J, Kunicka K, Graff B, Polonis K, Hoffmann M, Chrostowska M, Szyndler A, Bandosz P, Graff B, Narkiewicz K.Blood Press. 2018 Dec;27(6):376-384.
9. Impact of orthostatic hypotension and antihypertensive drug treatment on total and cardiovascular mortality in a very elderly community-dwelling population.
Szyndler A, Dereziński T, Wolf J, Narkiewicz K.J Hypertens. 2019 Feb;37(2):331-338
10. A multilocus genetic risk score is associated with arterial stiffness in hypertensive patients: the CARE NORTH study.
Polonis K, Hoffmann M, Szyndler A, Wolf J, Nowak R, Becari C, Laurent S, Boutouyrie P, Melander O, Narkiewicz K.J Hypertens. 2018 Sep;36(9):1882-1888
11. Central sympathetic nervous system reinforcement in obstructive sleep apnoea.
Wszedy’byl-Winklewska M, Wolf J, Szarmach A, Winklewski PJ, Szurowska E, Narkiewicz K.
12. Left ventricular ejection fraction and aortic stiffness are independent predictors of neurological outcome in acute ischemic stroke.
Rojek A, Gąsecki D, Fijałkowski M, Kowalczyk K, Kwarciany M, Wolf J, Nyka W, Boutouyrie P, Laurent S, Narkiewicz K.J Hypertens. 2016 Dec;34(12):2441-2448
CONTACT
- Prof. Dr. Habil. Krzysztof Narkiewicz
Chairman of the Scientific Council of the CMT
Translational Medicine Centre, Medical University of Gdańsk
Phone 58 349 2813
E-mail krzysztof.narkiewicz@gumed.edu.pl
- Dr. Habil. Jacek Wolf, M.D.
CMT Coordinator
Translational Medicine Centre, Medical University of Gdańsk
Phone 58 349 2813
E-mail jacek.wolf@gumed.edu.pl
- Magdalena Dzitkowska, Ph.D.
Translational Medicine Centre, Medical University of Gdańsk
Phone 58 349 2813
E-mail magdalena.dzitkowska@gumed.edu.pl
photo Paweł Sudara/MUG