Publication on elevated complement factor I expression in lung cancer cells
6.03.2024
Researchers at the Medical University of Gdańsk are co-authors of a publication titled Elevated expression of complement factor I in lung cancer cells associates with shorter survival – Potentially via non-canonical mechanism published in Translational Research (IF=7.8). The study was carried out in international cooperation with specialists from Spain, the Netherlands, Sweden and Norway.
The first author of the paper is Anna Felberg, Ph.D. from the Department of Cell Biology and Immunology at MUG, and other researchers from the same unit were involved in its development: Grzegorz Stasiłojć, Ph.D., Daria Kowalska, M.A., Alicja Kuźniewska, M.A. and Prof. Marcin Okrój, acting as Corresponding Author.
In addition, a team from the Department of Enzymology and Molecular Oncology at MUG contributed to the study: Zuzanna Polakiewicz, M.A., Kamila Kitowska, M.A. and Prof. Rafał Sądej as well as Kamil Myszczyński, M.A. of the Centre of Biostatistics and Bioinformatics Analysis and Michał Bieńkowski, Ph.D. of the MUG’s Department of Pathomorphology.
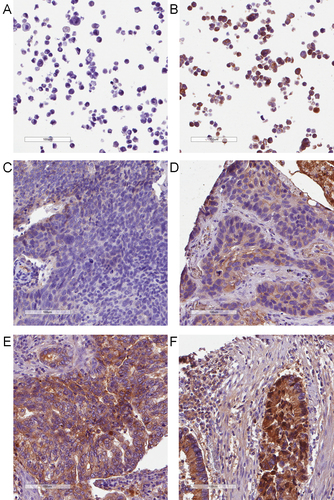
Fig. 1. Immunohistochemical staining of FI in lung cancer cell lines and tissue microarrays from lung cancer patients. Formalin-fixed paraffin-embedded (FFPE) pellets of lung cancer cell lines not expressing (A) and expressing (B) FI were used to setting up the staining parameters. The same conditions were applied to the staining of tissue microarrays generated from FFPE lung cancer tissues of patients. Pictures C-F show examples of lung cancer tissues scored as negative (-), positive (), strongly positive (+), and extremely positive (+), a measure that was further implemented in the H-score assessment.
 Fig. 3. Immunohistochemical staining of C4d. The staining was first validated in FFPE pellets of Raji cells sensitized with anti-CD20 antibody rituximab in FI-depleted serum (A) and the same serum reconstituted with FI (B). The same conditions were applied for the staining of normal lung tissue©, kidney transplant tissue showing antibody-mediated rejection (D) and lung cancer tissues from patients (E-F).
Fig. 3. Immunohistochemical staining of C4d. The staining was first validated in FFPE pellets of Raji cells sensitized with anti-CD20 antibody rituximab in FI-depleted serum (A) and the same serum reconstituted with FI (B). The same conditions were applied for the staining of normal lung tissue©, kidney transplant tissue showing antibody-mediated rejection (D) and lung cancer tissues from patients (E-F).
The authors noted a reduction in progression-free survival time in patients who had elevated expression of one of the complement system inhibitors, factor I (FI), in their tumor cells. In light of previous knowledge, the observation seemed to be a logical consequence of the expression of the inhibitor, which provides tumor cells with a greater degree of resistance to attack by the patient’s immune system, therefore the tumor grows and metastasizes faster. In order to confirm such a hypothesis, another immunohistochemical staining was performed in patient specimens, imaging the degradation product of the active complement component C4b – the C4d fragment, which is formed by FI activity. Surprisingly, no correlation was observed between the presence of the substrate (C4b), product (C4d) and enzyme carrying out the reaction (FI), suggesting a previously unknown reason for the observed poorer prognosis for patients. To explain the phenomenon, the researchers used the CRISPR/Cas9 genome editing technique and created clones of human lung cancer cells devoid of their natural FI expression.
RNA isolated from the cells was subjected to sequencing, and the results were subjected to bioinformatics analysis. In addition, FI-producing and FI-deficient cells were analyzed for signaling pathways after a cycle of temporarily eliminating serum from the culture medium and re-stimulating the cells with it. They also tested how both cell types performed in forming 3D colonies in a gel mimicking extracellular substance, isolated from any immune cells or dedicated activators of the complement system. The results showed that the mere presence or absence of FI in a cell significantly affects the expression of dozens of genes, including receptor genes for growth factors, genes controlling metabolism or the process of programmed death, and the presence of FI provides cells with an advantage demonstrated, e.g., in that they form large colonies faster and are less susceptible to cytotoxic compounds like etoposide.
– Until now, the complement system has been considered one of the mechanisms operating within nonspecific immunity. However, a very different, possibly primary function of this system is emerging from recent studies – namely, before it became the extracellular guardian of the organism over the course of evolution, it had a role in signal transduction inside the cell. Thus, it is very likely that another of the archaic aspects of the complement system function has been discovered, which in this case has a direct effect on the pulmonary cancer cell behavior – tsaid Prof. Marcin Okrój. – The translational potential of this discovery is that the precise identification of an element or slice of the complement cascade responsible for elevating the growth potential of cancer cells giving them better growth conditions (and thus a worse prognosis for the patient) would be a step toward effective adjuvant therapy. There is a number of drugs on the market that modulate the activity of the complement cascade, for which the safety profile, tolerable dose, pharmacokinetics, etc. are known, so possibly utilizing them for new indications would be much less challenging and expensive than developing a new drug from scratch..